- By Dr Richard Maurer
A few years ago, Jennifer came into my office for fatigue and perceived inability to lose weight. At the time she was 46 years old and her weight was normal on a BMI but she felt like her “belly was fat.” She felt like something was wrong and figured her doctor was missing something – just like when, after ten years of complaining, she was diagnosed with Ehlers-Danlos Syndrome (EDS).
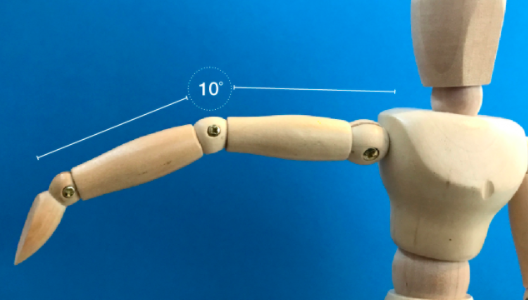
When I asked if the diagnosis of EDS helped her feel better: recover from injuries and tolerate exercise, she said no but it was helpful to know “that I wasn’t crazy.” The S in EDS stands for the word syndrome. Syndromes are ways physicians and fellow patients and researchers can talk about a condition without having to list off symptoms. But Ehler-Danlos does not lend itself to well to this. Beside the one common symptom of joint hypermobility related to collagen disruption, there are, as of early 2020, thirteen subtypes. https://www.ehlers-danlos.com/eds-types/ There are gene traits that are unique to these designations, yet some with a gene trait have no symptoms and others have significant EDS symptoms but do not carry the proper designated genetic variant. I have seen many patients over the years that have been diagnosed with EDS based upon symptoms but without genetic confirmation of the patient or a direct family member. Jennifer was one of those diagnoses.
Jennifer had already backed off strenuous exercise, but got more confused when friends chimed in. One family member said she must take turmeric to control inflammation, another friend said she should go paleo and eat more meat, yet another said going vegan would work.
The problem with this syndrome is particular – is the sheer variety. I am certain that many with the diagnosis of EDS have something different/additional going on. There are rare, severe types that can be life threatening yet most EDS cases are mild. As genetic science evolves, we will learn more about inheritance and progression of the collagen disease. If a direct line family member has been genetically diagnosed this is a pretty good chance that the symptoms of hypermobility and recurrent injury are related to EDS. So I don’t repeat accurate information on diagnosis and symptoms of EDS, I will steer you to the best link here: https://www.ehlers-danlos.com/eds-diagnostics/
To confirm an EDS diagnosis, I suggest following up with a genetic specialist that is familiar with the latest diagnostic criteria for the diagnosis. But in addition, I recommend getting some functional tests that give insight about collagen and soft tissue breakdown and associative recovery. This is metabolic performance recovery 101. When I said to Jennifer that I wanted her to do a test panel that was geared toward peak performance exercisers and athletes, she laughed. “I only work out in the pool with the 70-year-olds.”
I will list the Panel contents here for anyone to do…but essentially it covers the following, and then some more…[YOU CAN GET THIS PANEL IN THE U.S. through this link]
• C-reactive protein (CRP) and total WBC count to indicate inflammation that contributes to the breakdown of tissue. I have found that most people who think they have an inflammation problem, don’t. Rather, it is the lack of recovery that is the primary issue.
• Cortisol, Testosterone and DHEA – these stress/sex/anabolic hormones balance the stress/anxiety/breakdown state of the body (cortisol) with the rebuild process (testosterone and dhea)
• The CK enzyme indicates the load of muscle breakdown while the Prealbumin and total protein display whether protein is available for rebuild.
• B12, vitamin D and iron (as ferritin) are nutrients involved in rebuilding soft tissue and collagen. [I MUST ADD HERE, FERRITIN IS THE #1 DEFICIENCY I HAVE FOUND, that, when corrected,offers dramatic and even life altering improvement.]
• HgbA1c, Glucose, Insulin with fasting triglyceride:Hdl-Cholesterol (TG:HDL) all indicate metabolic breakdown and storage. From the fats and carbs you are eating—are you storing too much or conversely are you breaking down too rapidly? Typically with connective tissue breakdown, I do not want to see excess metabolic catabolism, aka breakdown. Breakdown of the body is indicated by LOW HgbA1C (<5.0%), LOW INSULIN (<2), TG of <40mg/dL or a TG:HDL ratio of <0.5.
When we reviewed Jennifer’s lab work, there was deficiency all over the place. Her “total protein” was 5.9 (below normal) and her total vitamin D was also low at 21. Her TG was 34 and her insulin measured <2—both low. Why was she feeling overweight? I supposed it to be a breakdown of muscle mass and her stomach was actually “lax/deconditioned” not “fat”. Getting her nutrition corrected helped. We used target supplementation and improved her diet to include 1) some slow carbs like potato and rice 2) animal fats for natural vitamin D and K2 and 3) higher and denser protein intake. Within 3-4 months, she had strength to withstand workouts that she had only successfully done in her teens and early 20’s. Realize Jen is only one subgroup of EDS patients and perhaps her diagnosis is in question, but I have used this same testing on people with all levels of confirmed EDS and improvement of the surrounding nutritional, hormonal and inflammatory environment always helps, of course to varying degrees.

I work with these values every day all day, but there is enough available written material where you can run the panel, then look at those results that are out of range and see if there are effective places to make changes. It is true that a higher protein diet with additional collagen and adequate nutrients like those found in the core nutrition program at my office (at least 20 mg zinc, B12 in active form at 500 mcg, vitamin D with vitamin K, plenty of magnesium, etc) helps most people. But more important is to get insight as to what is going on behind the curtain. Like in the Wizard of Oz, sometimes things are not what they seem when we pull the curtain back.
For more info, you can always get a copy of the book, The Blood Code and better understand the metabolic and thyroid components of the thorough Inflammation, Exercise, Performance and Recovery panel.



Comments are closed.