Learn why your Forced Expiratory Volume (FEV) can display your likelihood of death from many viruses, not just COVID-19…and what to do to improve it.
Conquer your CoMorbidities…part 2. My earlier report on Co-morbidity and COVID is here. highlighted the supplements I like assure to prevent cold and flu complications: https://thebloodcode.com/cold-and-flu-protocol-2020
[If you find these emails helpful – please spread the word, others can sign up for future emails at the homepage here]
It’s not just the virus.
I know, we’ve heard frequent news reports about someone in their 40’s who was “totally healthy” and then died with Covid-19 infection. There are clearly tragic cases…they are hard medically and emotionally but are fortunately rare and in the news because they are rare—something that occurs that was 95% likely is not newsworthy.
So what is the 95% story?
We have enlightening research that tells us what causes the complications and death in 90% of all the COVID cases that presented to medical setting for PCR testing. And it is easy to conclude that if less symptomatic and asymptomatic individuals who were never tested in the US were included in this data, the heart / lung / obesity link would be accurate to predict well over 95% of all adverse outcomes to COVID infection in all ages.
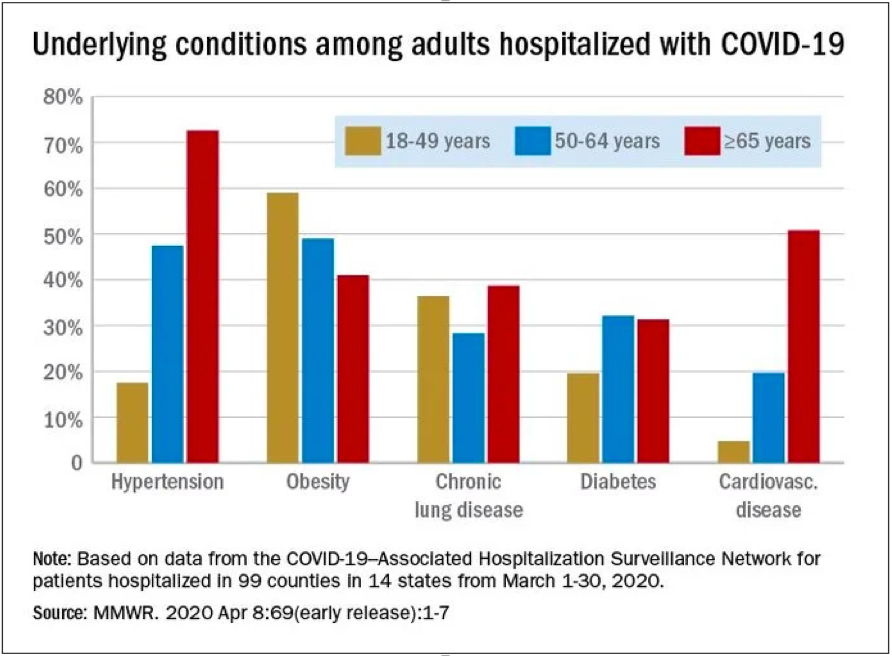
The RESEARCH: Recent data from a COVID-NET surveillance study that represents 14 states and about 10% of the US population finds that about 90% of all deaths due to COVID-19 occurred in people with one or more comorbid conditions. Further, in those over 65, the link was closer to 95%, mostly hypertension, and those younger than 65 had comorbid conditions 85% of the time, mostly obesity.
COVID-19 is remarkably non-fatal to kids. As of April 3rd, the US CDC reports three deaths in those under 18, and these deaths are yet unconfirmed as caused by COVID, all had underlying medical conditions. For comparison, the US CDC reported on April 4th that Influenza A and B strains have resulted in 166 deaths in children during this winter season thus far.
Simply, how do we get our adult bodies to behave more like we did as teenagers? The best current scientific explanation is microscopic—Young active immune systems and elevated ACE2 receptor activity, but let’s leave the deep science aside for now.
Since I am a Doctor that loves to find metrics that help answer questions about our health, I’d ask, “Is there some test that can display whether we are in that 5-10% high risk group and CAN that lab result be modified?
Enter FEV. Respiratory professionals use the full test name which is FEV1/FVC stated as FEV1%.
“FEV1 is the amount of air you can force from your lungs in one second. (measured by forcefully breathing out into a mouthpiece connected to a spirometer machine) and the FVC is simply the total lung capacity that can be forcefully breathed out (FVC). FEV1% is the amount breathed out in 1 second expressed as a percent of the total. IF you can breathe out >85-90% of your forced vital capacity in 1-second…you’re good! Obstructive Pulmonary Disease is measured as the FEV1% declines, <80%/<75%/<50%/etc.”
If you want to geek out on the metrics, medical spirometry equipment is a couple thousand dollars, but home kits with new technology are <$100-.
You could also keep it simple and optimize your FEV1% starting today bu doing TWO things, well one if you already have #1.
1 – The # 1 reason for a reduction in FEV1 is…SMOKING! This link is not subtle. Cause and effect is striking. And this links directly to coronavirus deaths, smoking is a fast way to get yourself in the small and exclusive high risk category for COVID-19 infection. The universe has dropped another reason to stop smoking.
2 – HIIT: Do demanding strenuous aerobic activity regularly. Check this study out…HIIT workouts three days a week for ONLY THREE WEEKS, significantly improved the FEV1 in deconditioned subjects. Since a significant number of you readers will be getting this infection in the next months to year, NOW is the best time to kick yourself into HIIT workouts a few days a week. This study started slower and made the workouts longer each week. http://biomedpharmajournal.org/vol11no2/the-effect-of-high-intensity-aerobic-exercise-on-the-pulmonary-function-among-inactive-male-individuals/

Reports from many professional athletes state how they had no symptoms at all but tested positive, other people I now have reported a marked shortness of breath with COVID-19 infection. We need to develop the best capacity and function of our lungs on a regular basis – like the best athlete relative to our individual baseline. Walking and long distance running work to increase the FVC, or the lung volume, but not the function or FEV1%.
THAT requires the HIIT workouts &I wrote about how I do these workouts here.
Yours in health,
Richard


Comments are closed.